Residency
- Residency Program Overview
- Message from the Residency Program Director
- How to Apply
- Residents
Our residency program offers trainees a balanced learning experience in a variety of leading-edge clinical facilities under the guidance of our distinguished faculty. Residents receive graduated caseloads, responsibilities and opportunities as their medical knowledge and clinical skills develop each post-graduate year (PGY), balancing participation in research and didactic education.

We are proud to offer residents the option to select from two training tracks:
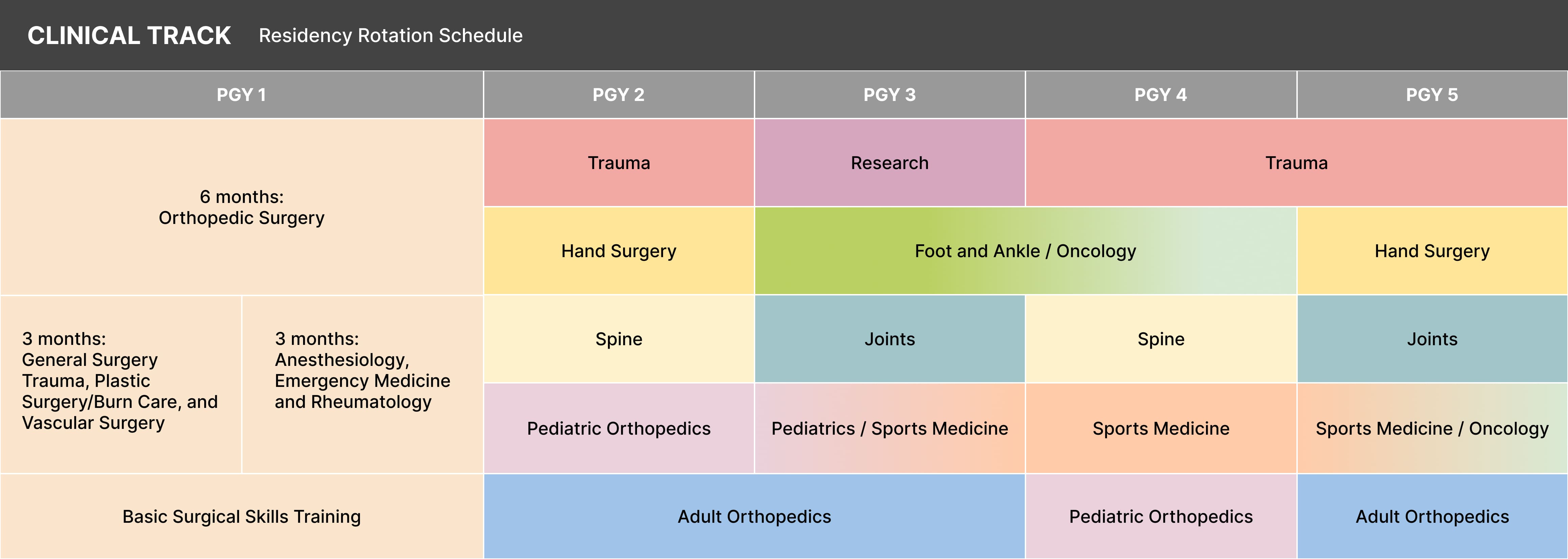
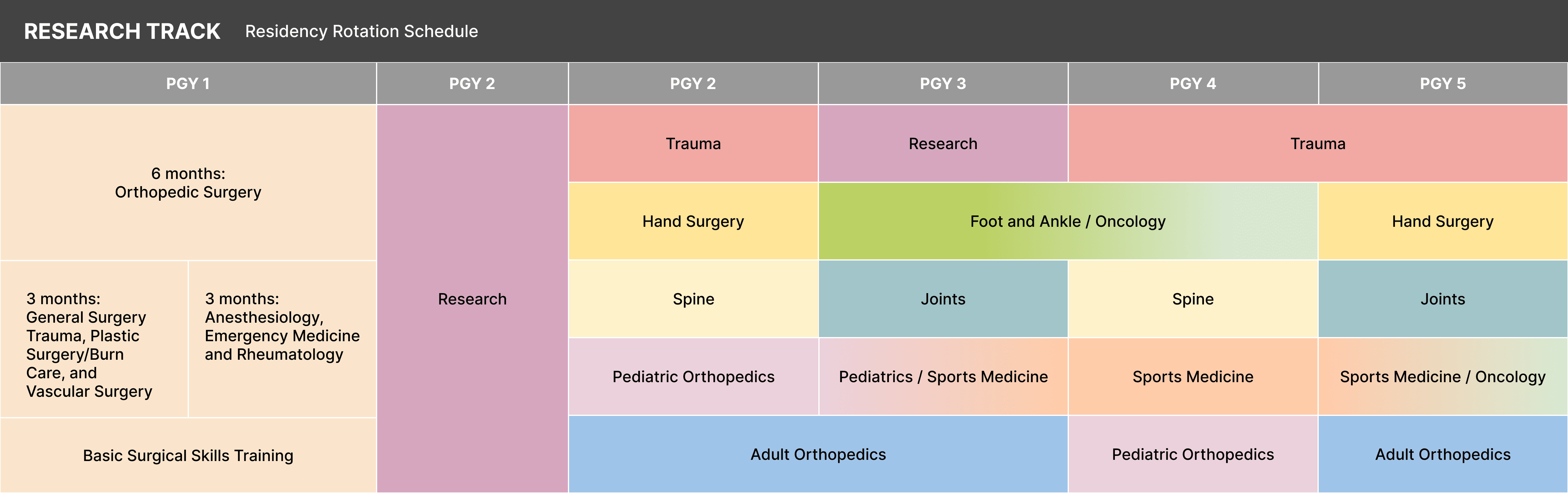
Each year our program matches four residents to the five-year clinical track and one resident to the six-year research track. During PGY 1, residents complete 6 months of orthopedic rotations and 6 months of non-orthopedic rotations; for the remaining PGYs, the rotations generally occur in 10–11-week blocks. In every facet of our mission, we uphold CARES values—Compassion, Accountability, Respect, Excellence and Service—with patients and visitors, as well as the academic community and our team.
Please note: Track schedules serve only as a guide and are subject to change based on the needs of the program and ACGME requirements.
Our mission is to educate a surgeon into becoming a knowledgeable and respected academic leader in leading-edge surgical methods and techniques by immersing them in scholarly pursuits and actively participating in research. The clinical track resident will engage in a wide variety of training opportunities in ambulatory, in-patient and operating room settings, while exposed to the full range of our department's subspecialties, from Joint Reconstruction to Spine Surgery.
Residents have access to multiple training facilities including operating rooms with a high-volume caseload. Embodying the institution's history of innovation, the clinical training program supplements its foundation in evidence-based clinical practice with opportunities to participate in research projects.
The research track resident will follow the same clinical training schedule as residents completing the five-year clinical track but will spend one year after their PGY 1 dedicated to conducting clinical, translational or basic research in our laboratory space. The resident has input into planning as well as performing projects for their research year.
Critical analysis of research literature, research techniques, statistical tools and regulatory requirements are emphasized. By the end of their research year, residents are expected to make meaningful contributions to the field of orthopedic literature, serving as a springboard for a career as a clinician-scientist.
We are committed to giving trainees resources that empower them to lead a fulfilling career in orthopedics within a wide range of disciplines. Additionally, appreciating the importance of nurturing a healthy work-life balance, we offer trainees numerous opportunities to balance wellbeing with their rigorous training schedule, including:
Residents will learn the material science of prosthetic joint replacement, indications for surgical treatment for adult hip and knee disease, and surgical anatomy for multiple surgical approaches. They are also provided with unique exposure to biological reconstruction, including osteotomy and osteocartilaginous transplantation. The rotation focuses on developing technical proficiency in the performance of basic hip and knee reconstructive procedures, recognizing patterns of prosthesis failure and understanding the basic concepts and details of rehabilitation after joint reconstructive procedures and the use of clinical pathways in patient care.
Residents will understand the pathophysiology of adult hip and knee diseases, including osteoarthrosis inflammatory arthrosis, traumatic arthrosis and avascular necrosis, as well as other cartilage diseases. In addition, residents will recognize the principles of prosthesis fixation and biological reaction to the prosthesis and design engineering principles underlying total joint replacement.
During the adult orthopedics rotation, residents are exposed to a wide variety of orthopedic pathologies with a large caseload volume of arthroplasty, sports medicine, shoulder pathology, and fractures. Residents learn about the diagnosis and treatment of adult orthopedic patients, gaining experience for establishing an appropriate diagnosis for each patient by the process of history taking and physical examination.
They will propose therapy plans for operative and non-operative care and assist with coordinating such therapy to its satisfactory conclusion.
Residents will participate in patient care responsibilities in inpatient and outpatient settings, including operating rooms, while developing an organized approach to the evaluation and treatment of foot and ankle conditions. Residents are exposed to a variety of conditions, including fractures, the diabetic foot, tendon issues, deformity, neuromuscular disorders and post-traumatic arthritis. They will be exposed to total ankle replacement, ankle arthroscopy, ligament repair, tendon transfers and complex deformity correction.
Emphasis during the rotation is on expanding the resident’s understanding of biomechanics and pathophysiology of foot and ankle disorders and developing clinical and surgical skills to evaluate and manage operative and non-operative conditions.
Residents will learn and be able to perform problem-oriented and nerve and motor specific examinations while learning the pathophysiology and treatment of common disorders of the upper extremities. They will become comfortable with basic science principles and clinical practice of hand surgery, including overuse syndromes, compressive neuropathies, soft tissue tumors and cysts, infections and septic joints, and congenital and acquired disorders. Residents will understand, and be proficient at, the non-operative and operative management of fractures, including the indications for replantation and both elective and acute management of upper extremity pathologies. Experience will be provided in the treatment of tendon and nerve lacerations, disabilities associated with nerve palsy and basic tendon transfers to restore function.
Residents will learn about the care and treatment of benign and malignant bone and soft tissue tumors, along with metastatic tumors involving the extremities, spine and pelvis. Residents will develop their surgical skills and understanding of techniques to manage soft tissue reconstruction, bony reconstruction, rotation flaps, wound vacs, skin grafts and complex wound closures.
Residents will learn the importance of, and schedules for, long-term surveillance of common bone and soft tissue tumors while gaining an understanding of staging protocols for specific conditions. Due to the nature of the oncology service, collaboration with other surgical teams is required.
Residents will learn the basic science principles of clinical practice in orthopedic sports medicine while developing the clinical and surgical skills needed to provide excellent arthroscopic and sports medicine care. Focus is on the evaluation and treatment of shoulder and knee disorders, with particular emphasis on basic and advanced arthroscopic surgical techniques.
Residents will understand commonly treated disorders, including shoulder instability and superior labral (SLAP) tears, impingement syndrome and rotator cuff tears, glenohumeral arthrosis, adhesive capsulitis, meniscus tears and knee chondrosis, knee instability, patellofemoral disorders, sports-related overuse syndromes, stress fractures and chronic exertional compartment syndrome.
UC San Diego Health is the official health care provider for the San Diego Padres, San Diego Seals and UC San Diego Athletics. In addition to these partnerships, potential training opportunities may exist with Balboa Naval Medical Center along with athletic training room responsibilities at local high schools and UC San Diego Athletics.
Because UC San Diego Hillcrest Medical Center is designated as a Level 1 trauma center, residents will receive a high level of exposure to the treatment of open and closed fractures, dislocations of the extremities and the management of multiple traumatized patients. Residents will participate in formulating diagnosis and treatment plans of bone, joint, muscle, nerve and other soft tissue injuries of the extremities, as well as a variety of infectious processes, possibly including septic joints, osteomyelitis, and soft tissue infections such as cellulitis, necrotizing fasciitis, gas gangrene and abscess.
Residents will have abundant opportunities in non-operative and operative treatment of pediatric orthopedic conditions and gain insight into numerous subspecialties, including spine and scoliosis, pelvic osteotomies, sports, and foot and ankle. Residents will learn to diagnose and treat all common pediatric orthopedic surgery problems and develop basic operative skills related to pediatric orthopedics, including treatment of closed and open fractures, and aspiration and surgical drainage of suspected infections.
During the rotation, they will also participate in, and be exposed to, complex pediatric orthopedic operations, involving surgical treatment of scoliosis, congenital dislocation of the hip, and Legg-Calve-Perthes disease. Residents will learn the affective components of being a physician, including good inter-professional and doctor-patient skills.
Residents will learn and understand cervical, thoracic, and lumbar spine anatomy and develop an organized approach to evaluation and treatment of spine-injured patients intact, incomplete, or complete and assess spinal stability and instability. Residents will participate in the evaluation of patients in the clinic setting with a variety of complaints, including back, leg, neck, and arm pain as related to degenerative conditions, tumor, infections, spondyloarthropathies and deformities. Residents will improve their surgical techniques and understand the rationale and indications for using spinal orthoses. Residents may participate in non-operative and operative care for patients at the Veteran Affairs Medical Center and the Veteran Affairs Spine Cord Injury Unit in a consultative manner.